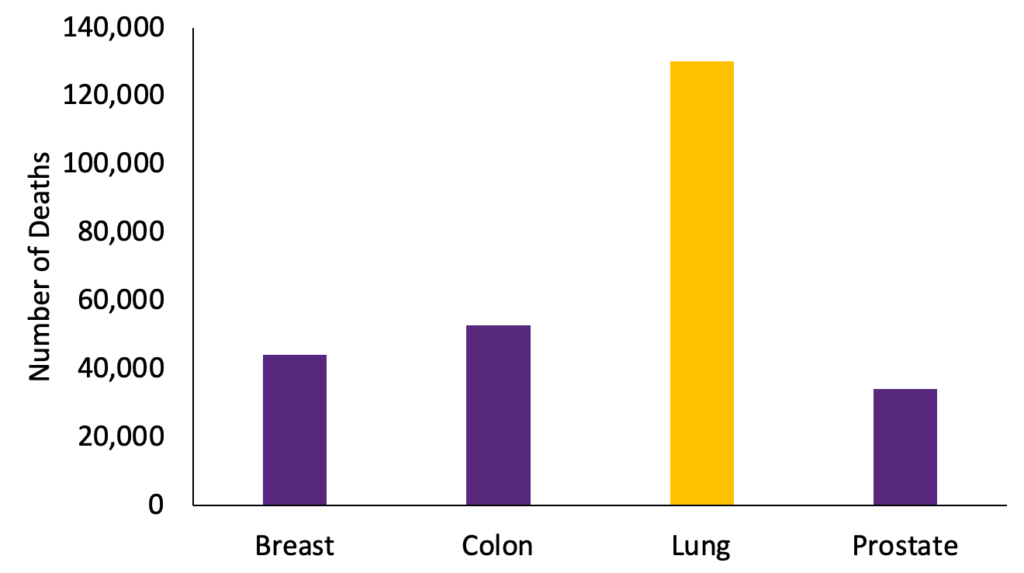
Lung cancer causes more deaths every year than breast, colon, and prostate cancer combined. This is mainly because nearly half of all lung cancer is diagnosed once it has already spread. When diagnosed at this stage, less than 7% of lung cancer patients survive for more than 5 years after their diagnosis.
Lung cancer screening with a low-dose computed-tomography (LDCT) scan can save countless lives by catching lung cancer early, when it is most treatable. When lung cancer is caught early, almost 60% of patients survive for at least five years after their diagnosis. The survival rate for early-stage lung cancer is over 8 times better than the survival rate for late-stage lung cancer.
The landmark National Lung Cancer Screening Trial (NLST) published in 2011 showed that annual lung cancer screening with LDCT reduced lung cancer mortality by 20% when compared to chest x-ray. The Nederlands–Leuvens Longkanker Screenings Onderzoek (NELSON) trial published in 2020, showed that annual screening with LDCT reduced lung cancer mortality by 24% in males and 33% in females.
These trials produced the evidence for the current United States Preventive Services Taskforce (USPSTF) lung cancer screening guidelines. Lung cancer screening with a LDCT scan is now recommended and covered by insurance for patients who meet the following criteria:

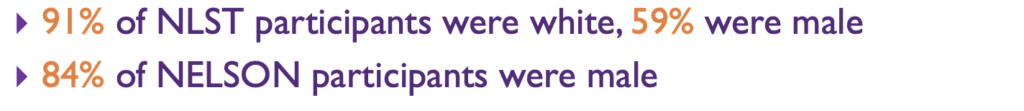
While both the NLST and the NELSON trials showed the exceptional benefit of lung cancer screening in high-risk populations, the majority of patients were White and Male.
Due to the lack of racial and sex diversity in the trials that provided evidence for the USPSTF guidelines, the current guidelines exclude many non-white and non-male patients who are at high-risk for lung cancer. Black women are most likely to be ineligible for lung cancer screening, even when they are at high risk of lung cancer.
In retrospective analyses of the Southern Community Cohort Study (SCCS) and the Black Women’s Health Study (BWHS), our team led by Alex Potter and Dr. Yang, found that less than half of Black women who were diagnosed with lung cancer would have been eligible for lung cancer screening under the current USPSTF guidelines. On the other hand 75% of white women would have been eligible for lung cancer screening.
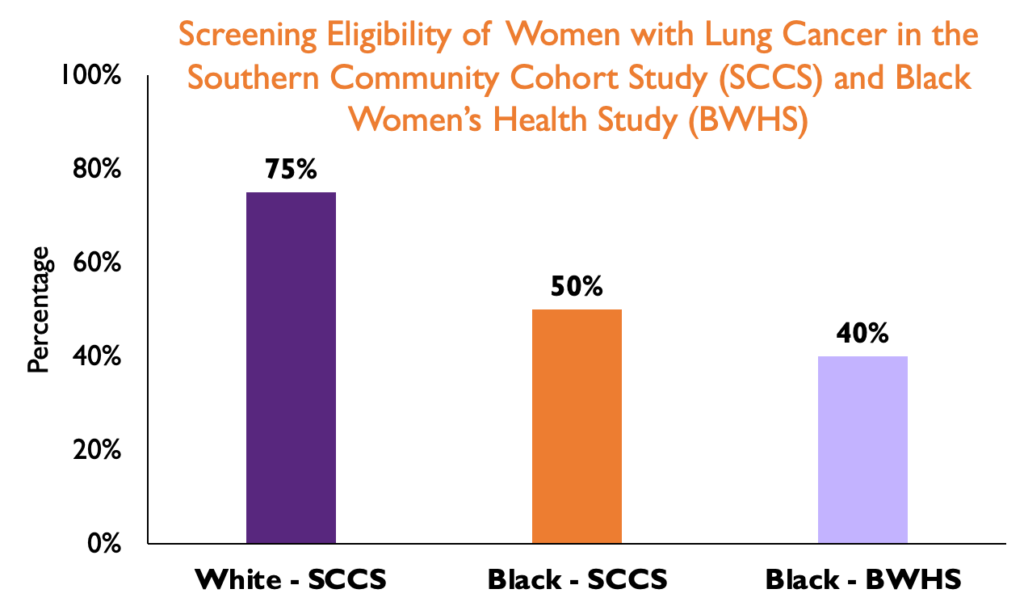
When we looked into why these disparities occur, we found that Black women diagnosed with lung cancer have a lower pack-year smoking history despite having smoked for a similar amount of time as White women diagnosed with lung cancer. This causes many high-risk patients to be ineligible for lung cancer screening because they have not smoked enough to meet the 20 pack-year requirement.
Notably, disparities in screening eligibility in the SCCS and the BWHS would be eliminated if the 20 pack-year smoking requirement were to be replaced with a 20-year smoking duration requirement.
Through the INSPIRE study, we will prospectively study the performance and feasibility of screening Black women with a smoking history who would not be eligible for lung cancer screening under the USPSTF guidelines in addition to those who are currently eligible. We will study how the 20-year duration requirement performs in identifying patients at high-risk for lung cancer compared to the 20 pack-year requirement. We will also explore how AI tools can be utilized to predict lung cancer risk. Ultimately we hope to identify novel solutions that improve opportunities for early detection among Black women at high-risk for lung cancer.
